The human body is made up of all sorts of shapes and sizes of bones, ligaments, muscles, organs and tissue, almost none of which are flat. Yet most X-ray scanners are flat and rigid. But that is all set to change, with a new generation of X-ray technology – based on semiconductor ink – about to make it possible to create curved detectors that fit around different parts of the body.
It may even be possible to individually customise these using low-cost flexible printed electronics for personalised patient care, with better outcomes for patients worldwide.
The primary reason for using flat radiographs is historical. Black-and-white analogue photography relies on the photosensitive nature of film. The structure of this film, when exposed to light, is invisibly modified as photoelectrons are liberated from the silver halide crystal and proceed to form a metallic silver speck which grows with extended exposure.
Once exposed, the film can be fixed and developed onto photosensitive paper in a dark room. The inherent consequence of this exposure process is that both the film and the photographic paper must be held flat and parallel to each other to avoid distorting the image. Consequently, although the film itself is flexible, the process that is used to produce photos or radiographs from the exposed film means it can only practically be used flat.
Since the early 2000s, newer digital flat-panel X-ray detectors have replaced a large segment of the radiography film market, as they offer the ability to see digital X-ray images on screen immediately, without the time-consuming post-processing step required for radiographic film.
However, these have introduced a further limitation to the rigid nature of detectors, as the electronic circuits used to capture and digitise the images are fabricated using the same basic technology as displays, such as TVs and computer monitors, which are typically designed with thin film electronics printed on glass backplanes. For higher-performance X-ray imaging (higher resolution, faster speeds), newer CMOS process technology is used, with the electronic backplanes designed as ASICs on silicon wafers, using the same image sensor designs as camera phones.
With the introduction of curved display monitors, foldable mobile phone screens and flexible electronics in industrial applications, it finally opens the door to a move away from the restrictions of flat electronics for medical imaging to ones that can be shaped to fit around the body.

Above: Example of a medical X-ray setup with Flat Panel Detector (Digital Radiography)
The X-ray conversion layer
In addition to the electronics which capture, store and digitise the signals into a pixelated image, there is another critical component within every X-ray detector – the X-ray conversion layer. This layer converts X-rays into signals that the electronics can understand and process. The most common conversion layer is a scintillator, which converts the X-rays into light. The electronics have an integrated photodiode within the circuit for each pixel to convert the light that is emitted by the scintillator into an electronic charge which can be stored, in the same way a digital camera works. This type of digital X-ray detector is known as an ‘indirect’ detector as it uses a two-stage conversion process: X-rays to light (conversion stage 1), then light to electronic charge (conversion stage 2).
Scintillators can deliver very good image clarity (resolution), but this comes at the expense of conversion efficiency (X-ray dose or flux). To achieve good image clarity, the scintillator must be as thin as possible – no more than twice the underlying pixel resolution – to avoid light being absorbed by pixels adjacent to the one that was exposed by the initial X-ray that was converted to light. As the scintillator thickness is increased, there is a significant loss of image clarity, as the light scatters in all directions throughout the scintillator layer and will be incorrectly captured in adjacent pixels, thereby causing the image to be blurred.
Conversely, to make a high-efficiency detector (meaning the ability to capture and use every X-ray rather than only a proportion of them), the scintillator should be made as thick as possible. This is because the conversion efficiency is defined by the quantity of X-rays that the scintillator layer will absorb for a given X-ray energy, which is proportional to the conversion material’s density and atomic number.
To manage this trade-off, scintillators for medical detectors are typically thick (for example, 600 µm), to keep the radiation exposure for patients as low as possible but with relatively poor image quality, whereas scintillators for high-resolution industrial detectors, such as the inspection of electronic assemblies, are typically much thinner – for example, 150 µm. Considering the thicknesses required for medical applications, this introduces a further limitation for flexible detectors, where the total thickness of the stack (conversion layer plus electronics) should be in the order of 100 µm to remain conformable.
Thanks to a recent breakthrough in X-ray semiconductor ink technology, a new thin film material with high conversion efficiency is showing promise as an alternative option compared with traditional scintillators for the X-ray conversion layer. This material is a ‘direct’ conversion material, converting X-rays directly into electronic charge, without needing to go through the light conversion step. Considering the high efficiency of the material, a much thinner layer is required, thereby removing the need to trade off dose against image quality, while also being able to deliver a sufficiently thin layer to produce flexible detectors.
So, what could the future look like, if flexible electronics, combined with thin high-efficiency X-ray conversion materials (semiconductor inks), could be used to develop conformable X-ray detectors?
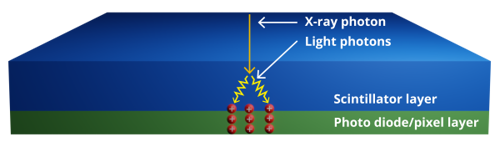
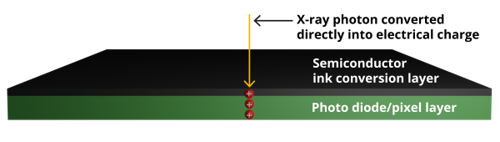
Above: The first figure shows existing 'indirect' conversion X-ray detectors that use a scintillator layer to convert X-rays to light first. The more efficient 'direct' conversion detectors, in the image below, convert X-rays to electrical charge with a thin semiconductor ink layer
More accurate radiotherapy with fewer side effects
In radiotherapy, preservation of healthy tissue is of the utmost importance while treating the tumour - sparing organs which are particularly sensitive to radiation or where loss of function may occur – for example, in the brain.
Radiotherapy is used in 40% of cancer treatments and a challenge is ensuring the accuracy of these treatments when performed by medical physicists in the treatment facility. Treatment plans are optimised to minimise the radiation dose to sensitive areas of the brain which are fundamental to hearing, eyesight and memory.
Three immediate benefits would be possible with flexible digital X-ray film:
- Currently, only one in 20 patient plans for Gamma Knife treatment are checked for quality monitoring due to the cumbersome process of using radiographic film, digitising it and combining the data into a useable format. The frequency of the quality monitoring plans could be increased by simplifying and speeding up the process, with a direct benefit to patient health.
- By digitising existing sets of 2D films to produce a 3D image, the scanning step introduces errors and inaccuracies. With digital film, new ‘real-time’ 3D image resolution would improve, enabling the treatment plan to be checked in finer detail, leading to better patient outcomes.
- To ensure patients are positioned in line with a known reference to the radiotherapy treatment beam, a head frame is usually screwed into the patient’s skull to restrain them. With flexible X-ray detectors, a personalised skull cap with an embedded printed radiation detector on it could accurately monitor – and potentially even correct – the position of the treatment beam in real time.
Mammograms without compressing the breast
More than a million women in England missed out on vital breast cancer screening in 2021-22, according to the Breast Cancer Now charity. The prospect of undergoing a painful – or at least uncomfortable – mammogram can often be one of the reasons for women avoiding the vital screening.
With the advent of conformable digital X-ray film, it should be feasible to move away from flat detectors for mammograms to ones that can be shaped to fit around the breast. The discomfort reported by many women could then be eliminated as the breast would no longer have to be compressed to fit onto a flat-panel X-ray detector. Additionally, with the detector shaped around the breast, 3D images would provide better detection accuracy than traditional mammography detectors can currently achieve.

Above: Mammograms are performed by compressing the breast onto a flat X-ray detector to check for abnormalities
If the radiation dose could also be reduced while maintaining the same quality of image, with higher detector efficiency, the breast screening programme could also be offered at an earlier age. Several oncologists already advocate the concept of personalised breast cancer screening, according to a patient’s own unique health history and risk factors. A lower-dose mammography service would strengthen that approach.
In short, a personalised approach to the adoption of new X-ray detector technology would encourage a higher uptake of preventative scans, tailored towards patients with higher risk profiles – and detecting cancer at an earlier stage to ensure better patient outcomes.
Intra-oral dental X-rays without discomfort
Dental radiographs are valuable diagnostic aids for oral healthcare, and intra-oral examinations are commonly used by dental practices worldwide for routine checks or dental health, particularly for detection of caries and for examination prior to an extraction procedure.
However, some patients experience problems during intra-oral radiographic examinations due to their age, neurological issues or anatomical difficulties such as a large tongue, a shallow palate or restricted mouth opening. In addition, a significant number of patients are unable to tolerate the intra-oral film/sensor placement in their mouth due to the gag reflex. This number has increased with the advent of digital radiography because of the rigidity and thickness of the radiographic sensor. For this reason, many dental practices continue to use radiographic film – or simply elect not to X-ray at the practice, and instead refer them to a specialist orthodontal clinic where extra-oral X-rays can be taken.
For such cases, new dental X-ray detectors could be moulded to any tolerable shape. For example, a soft and flexible intra-oral detector with the consistency of a marshmallow would improve patient comfort, eliminate the gag reflex and improve dental hygiene for a wider spectrum of the population. In addition, with higher sensitivity, this could be achieved at a lower level of radiation exposure – of particular significance for younger children.
The key to success
New technology always hails a dawn of new opportunities. Many such opportunities come from the divergence of the status quo to a new way of thinking and embracing innovations. And each innovation will require several barriers to be overcome before they deliver on their promise. In this instance, the opportunities for flexible X-ray detectors are plentiful.
The key to success will be how well they can be actioned, delivered and embraced by a traditionally conservative practitioner community.
Author details: Dan Cathie is CEO of Silveray













